That is the question and it is the most important question you need to ask if you are moved from the emergency room to the hospital floor.
I knew to ask it but this last time around I was not able to pin the response down clearly enough. I live alone, have no family out here to be with me in the ER. although I can call upon family to talk with the doctors, they do not always call them back with these details. What is a person like myself supposed to do?
If there is time, the next time I think I need to go to the ER I am going to resume the habit I had when I was receiving intensive chemotherapy. I will contact the gynecologist on call or my primary doctor on call and get their assistance in the process. They can help communicate with the ER hospitalist and provide much needed confidence to the ER hospitalist so that an inpatient admission to the floor is what occurs if I am taken to the floor for treatment and testing. Medicare severely punishes hospitals for wrongly admitting a patient.
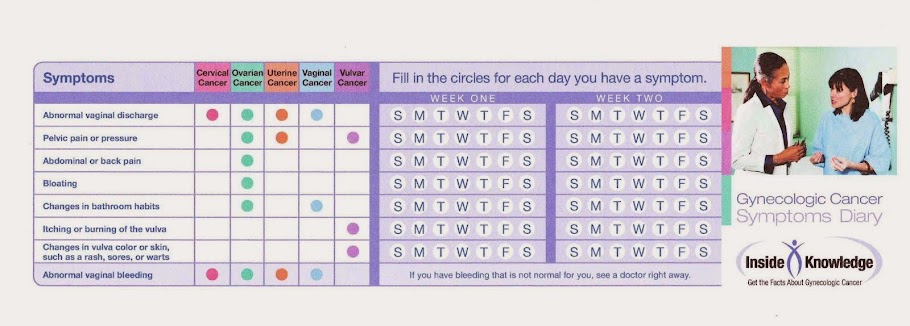
As a cancer patient I am more likely to go to the ER because of all of the side effects of current and past treatments received for ovarian cancer.
I spoke with an administrator at the hospital, thanks to the referral from my amazing hospitalist on the floor. The administrator shared with me that there is a 48 hour window, the 2 midnight rule, that does allow a hospitalist to change the status if there is substantial back up and great documentation. Also to note though is that if a person is admitted and they get better before the 2 midnight rule hits, then the documentation needs to add that the patient got better sooner than expected.
If this confuses you, you are not alone. Medicare has this new 2 midnight rule in place that requires an ER doctor to justify an admission by predetermining if a patient will be in hospital for more than 2 midnights. This is insane because time is not a dictator of treatment success. The ER doctor may or may not yet have that information which is why a patient needs admitted!
New laws are in place requiring hospitals to notify a patient of this status but not all hospitals are doing this yet. I was recently in the ER, had been moved to the floor, asked if I was admitted, told yes, but was admitted to observation. This is an oxymoron, there is no such thing as admission to observation. Observation is kind of a holding status. I had already received a CT scan and when I found out I was not an inpatient, as needed, I was very disheartened and upset.
If you hear the words "admission" "observation" "monitor" in the same sentence, BEWARE. I have always been an advocate for getting clarity about "observation status" for myself and others yet I fell into it anyway. I do not think any patient under the influence of IV pain meds or in a state of duress can be considered competent enough to decipher the code words for observation unless the words "you are an outpatient under observation" are branded on our hospital band, written on the communication board AND communicated to a caregiver or family member.
By the grace of God the hospitalist on the floor stood up for me, the patient. He asked hard questions and it was clear that I was an inpatient, my status corrected and I was provided assistance to get my situation clarified. Thank you Lord! Imagine though had I been totally confused for any reason. I would have had no way of knowing this until I received an outrageous bill for services not covered as an outpatient in observation. This happens to thousands of people per year.
For an in-depth look at this huge problem link to Hospital Medicine.org.
New laws are in place to require hospitals to notify patients with certainty as to their status, but not all hospitals are following the rules yet.
The Notice of Observation Treatment and Implication for Care Eligibility Act would require a written, explanation of the Medicare patient’s status as an outpatient under observation, why they are in that status, and outline the cost sharing and skilled nursing facility (SNF) implications.
http://www.hfma.org/Content.aspx?id=32889 Congress Passes Requirements for Observation Status Notification, Cost Assessments
RICH DALY, HFMA SENIOR WRITER/EDITOR
I personally believe the observation status option should be removed in its entirety and Medicare should enable doctors do what they need to do to help their patients. I am going to add my 2 cents and say we need a single payer system for everyone and get rid of all of this red tape that interferes with high quality care. Especially deceiving misleading red tape involving observation status.
When we are taken to the emergency room we do not have any idea as to if we will need any rehabilitative services. The outpatient status negates coverage of skilled nursing care, if such a need arises. Medicare beneficiaries also will not be covered for services provided in the hospital if the patient is under observation status, as opposed to inpatients.
Here are a few helpful links regarding observation status, its consequences and pending legislation to alleviate some of the resulting financial hardships that break the backs of medicare beneficiaries. If you have medicare advantage you could fall prey to this hardship as well. Please contact your insurance company. Do not make any assumptions.
http://www.modernhealthcare.com/article/20150520/NEWS/150529982 Medicare recovery audit program targeted for reform after spike in observation stays
By Helen Adamopoulos | May 20, 2015
S.843 — 114th Congress (2015-2016)
Improving Access to Medicare Coverage Act of 2015
http://www.medicareadvocacy.org/self-help-packet-for-medicare-observation-status/ Self Help Packet for Medicare
I am sorry to have imposed all of this information upon you because it is not uplifting. I just want to do all I can to help you to avoid falling into this loophole. The original intent of the observation status was to prevent fraud and its use has gotten out of hand hurting thousands of people, placing good doctors in a terrible position and costing hospitals huge fines and placing patients in financial hardship, possibly bankruptcy.
It is costly to manage, I imagine. Landsharks can be sent back to patients to recover money after an audit that has reversed a status from inpatient to observation. This ruins everything for these patients forcing them to lose savings, homes and assets that they have worked for all their life. It is just criminal in my mind.
Remember to ask up front if you are an Inpatient or an Outpatient! By the way, I am really knocked down. I live literally 50 feet fom my pharmacy/grocery store. When I walked across the parking lot to fill my prescription the staff gave me a free bottle of water, asked me to please sit down and told me I was very pale. I was breathing hard, very short of breath. I did not realize how weak I was. This evening I did not make it to church, as I desperately wanted. I am too tired and do not want to drive. I have not driven a car since October 14th. I have had my fill of hospitalizations for awhile.....ha.
I hope you find these resources helpful. It is a lot of information to swallow. I hope there are no typos, I am still very fatigued from my stay at the hospital. Happy November by the way.
Peace and Blessings!
Denise
Servivorgirl